- Research
- Open access
- Published:
Use of the International IFOMPT Cervical Framework to inform clinical reasoning in postgraduate level physiotherapy students: a qualitative study using think aloud methodology
BMC Medical Education volume 24, Article number: 486 (2024)
Abstract
Background
Vascular pathologies of the head and neck are rare but can present as musculoskeletal problems. The International Federation of Orthopedic Manipulative Physical Therapists (IFOMPT) Cervical Framework (Framework) aims to assist evidence-based clinical reasoning for safe assessment and management of the cervical spine considering potential for vascular pathology. Clinical reasoning is critical to physiotherapy, and developing high-level clinical reasoning is a priority for postgraduate (post-licensure) educational programs.
Objective
To explore the influence of the Framework on clinical reasoning processes in postgraduate physiotherapy students.
Methods
Qualitative case study design using think aloud methodology and interpretive description, informed by COnsolidated criteria for REporting Qualitative research. Participants were postgraduate musculoskeletal physiotherapy students who learned about the Framework through standardized delivery. Two cervical spine cases explored clinical reasoning processes. Coding and analysis of transcripts were guided by Elstein’s diagnostic reasoning components and the Postgraduate Musculoskeletal Physiotherapy Practice model. Data were analyzed using thematic analysis (inductive and deductive) for individuals and then across participants, enabling analysis of key steps in clinical reasoning processes and use of the Framework. Trustworthiness was enhanced with multiple strategies (e.g., second researcher challenged codes).
Results
For all participants (n = 8), the Framework supported clinical reasoning using primarily hypothetico-deductive processes. It informed vascular hypothesis generation in the patient history and testing the vascular hypothesis through patient history questions and selection of physical examination tests, to inform clarity and support for diagnosis and management. Most participant’s clinical reasoning processes were characterized by high-level features (e.g., prioritization), however there was a continuum of proficiency. Clinical reasoning processes were informed by deep knowledge of the Framework integrated with a breadth of wider knowledge and supported by a range of personal characteristics (e.g., reflection).
Conclusions
Findings support use of the Framework as an educational resource in postgraduate physiotherapy programs to inform clinical reasoning processes for safe and effective assessment and management of cervical spine presentations considering potential for vascular pathology. Individualized approaches may be required to support students, owing to a continuum of clinical reasoning proficiency. Future research is required to explore use of the Framework to inform clinical reasoning processes in learners at different levels.
Introduction
Musculoskeletal neck pain and headache are highly prevalent and among the most disabling conditions globally that require effective rehabilitation [1,2,3,4]. A range of rehabilitation professionals, including physiotherapists, assess and manage musculoskeletal neck pain and headache. Assessment of the cervical spine can be a complex process. Patients can present to physiotherapy with vascular pathology masquerading as musculoskeletal pain and dysfunction, as neck pain and/or headache as a common first symptom [5]. While vascular pathologies of the head and neck are rare [6], they are important considerations within a cervical spine assessment to facilitate the best possible patient outcomes [7]. The International IFOMPT (International Federation of Orthopedic Manipulative Physical Therapists) Cervical Framework (Framework) provides guidance in the assessment and management of the cervical spine region, considering the potential for vascular pathologies of the neck and head [8]. Two separate, but related, risks are considered: risk of misdiagnosis of an existing vascular pathology and risk of serious adverse event following musculoskeletal interventions [8].
The Framework is a consensus document iteratively developed through rigorous methods and the best contemporary evidence [8], and is also published as a Position Statement [7]. Central to the Framework are clinical reasoning and evidence-based practice, providing guidance in the assessment of the cervical spine region, considering the potential for vascular pathologies in advance of planned interventions [7, 8]. The Framework was developed and published to be a resource for practicing musculoskeletal clinicians and educators. It has been implemented widely within IFOMPT postgraduate (post-licensure) educational programs, influencing curricula by enabling a comprehensive and systemic approach when considering the potential for vascular pathology [9]. Frequently reported curricula changes include an emphasis on the patient history and incorporating Framework recommended physical examination tests to evaluate a vascular hypothesis [9]. The Framework aims to assist musculoskeletal clinicians in their clinical reasoning processes, however no study has investigated students’ use of the Framework to inform their clinical reasoning.
Clinical reasoning is a critical component to physiotherapy practice as it is fundamental to assessment and diagnosis, enabling physiotherapists to provide safe and effective patient-centered care [10]. This is particularly important for postgraduate physiotherapy educational programs, where developing a high level of clinical reasoning is a priority for educational curricula [11] and critical for achieving advanced practice physiotherapy competency [12,13,14,15]. At this level of physiotherapy, diagnostic reasoning is emphasized as an important component of a high level of clinical reasoning, informed by advanced use of domain-specific knowledge (e.g., propositional, experiential) and supported by a range of personal characteristics (e.g., adaptability, reflective) [12]. Facilitating the development of clinical reasoning improves physiotherapist’s performance and patient outcomes [16], underscoring the importance of clinical reasoning to physiotherapy practice. Understanding students’ use of the Framework to inform their clinical reasoning can support optimal implementation of the Framework within educational programs to facilitate safe and effective assessment and management of the cervical spine for patients.
Objective
To explore the influence of the Framework on the clinical reasoning processes in postgraduate level physiotherapy students.
Methods
Design
Using a qualitative case study design, think aloud case analyses enabled exploration of clinical reasoning processes in postgraduate physiotherapy students. Case study design allows evaluation of experiences in practice, providing knowledge and accounts of practical actions in a specific context [17]. Case studies offer opportunity to generate situationally dependent understandings of accounts of clinical practice, highlighting the action and interaction that underscore the complexity of clinical decision-making in practice [17]. This study was informed by an interpretive description methodological approach with thematic analysis [18, 19]. Interpretive description is coherent with mixed methods research and pragmatic orientations [20, 21], and enables generation of evidence-based disciplinary knowledge and clinical understanding to inform practice [18, 19, 22]. Interpretive description has evolved for use in educational research to generate knowledge of educational experiences and the complexities of health care education to support achievement of educational objectives and professional practice standards [23]. The COnsolidated criteria for REporting Qualitative research (COREQ) informed the design and reporting of this study [24].
Research team
All research team members hold physiotherapy qualifications, and most hold advanced qualifications specializing in musculoskeletal physiotherapy. The research team is based in Canada and has varying levels of academic credentials (ranging from Clinical Masters to PhD or equivalent) and occupations (ranging from PhD student to Director of Physical Therapy). The final author (AR) is also an author of the Framework, which represents international and multiprofessional consensus. Authors HG and JS are lecturers on one of the postgraduate programs which students were recruited from. The primary researcher and first author (KK) is a US-trained Physical Therapist and Postdoctoral Research Associate investigating spinal pain and clinical reasoning in the School of Physical Therapy at Western University. Authors KK, KH and PP had no prior relationship with the postgraduate educational programs, students, or the Framework.
Study setting
Western University in London, Ontario, Canada offers a one-year Advanced Health Care Practice (AHCP) postgraduate IFOMPT-approved Comprehensive Musculoskeletal Physiotherapy program (CMP) and a postgraduate Sport and Exercise Medicine (SEM) program. Think aloud case analyses interviews were conducted using Zoom, a viable option for qualitative data collection and audio-video recording of interviews that enables participation for students who live in geographically dispersed areas across Canada [25]. Interviews with individual participants were conducted by one researcher (KK or KH) in a calm and quiet environment to minimize disruption to the process of thinking aloud [26].
Participants
AHCP postgraduate musculoskeletal physiotherapy students ≥ 18 years of age in the CMP and SEM programs were recruited via email and an introduction to the research study during class by KK, using purposive sampling to ensure theoretical representation. The purposive sample ensured key characteristics of participants were included, specifically gender, ethnicity, and physiotherapy experience (years, type). AHCP students must have attended standardized teaching about the Framework to be eligible to participate. Exclusion criteria included inability to communicate fluently in English. As think-aloud methodology seeks rich, in-depth data from a small sample [27], this study sought to recruit 8–10 AHCP students. This range was informed by prior think aloud literature and anticipated to balance diversity of participant characteristics, similarities in musculoskeletal physiotherapy domain knowledge and rich data supporting individual clinical reasoning processes [27, 28].
Learning about the IFOMPT Cervical Framework
CMP and SEM programs included standardized teaching of the Framework to inform AHCP students’ clinical reasoning in practice. Delivery included a presentation explaining the Framework, access to the full Framework document [8], and discussion of its role to inform practice, including a case analysis of a cervical spine clinical presentation, by research team members AR and JS. The full Framework document that is publicly available through IFOMPT [8] was provided to AHCP students as the Framework Position Statement [7] was not yet published. Discussion and case analysis was led by AHCP program leads in November 2021 (CMP, including research team member JS) and January 2022 (SEM).
Think aloud case analyses data collection
Using think aloud methodology, the analytical processes of how participants use the Framework to inform clinical reasoning were explored in an interview with one research team member not involved in AHCP educational programs (KK or KH). The think aloud method enables description and explanation of complex information paralleling the clinical reasoning process and has been used previously in musculoskeletal physiotherapy [29, 30]. It facilitates the generation of rich verbal [27]as participants verbalize their clinical reasoning protocols [27, 31]. Participants were aware of the aim of the research study and the research team’s clinical and research backgrounds, supporting an open environment for depth of data collection [32]. There was no prior relationship between participants and research team members conducting interviews.
Participants were instructed to think aloud their analysis of two clinical cases, presented in random order (Supplementary 1). Case information was provided in stages to reflect the chronology of assessment of patients in practice (patient history, planning the physical examination, physical examination, treatment). Use of the Framework to inform clinical reasoning was discussed at each stage. The cases enabled participants to identify and discuss features of possible vascular pathology, treatment indications and contraindications/precautions, etc. Two research study team members (HG, PP) developed cases designed to facilitate and elicit clinical reasoning processes in neck and head pain presentations. Cases were tested against the research team to ensure face validity. Cases and think aloud prompts were piloted prior to use with three physiotherapists at varying levels of practice to ensure they were fit for purpose.
Data collection took place from March 30-August 15, 2022, during the final terms of the AHCP programs and an average of 5 months after standardized teaching about the Framework. During case analysis interviews, participants were instructed to constantly think aloud, and if a pause in verbalizations was sustained, they were reminded to “keep thinking aloud” [27]. As needed, prompts were given to elicit verbalization of participants’ reasoning processes, including use of the Framework to inform their clinical reasoning at each stage of case analysis (Supplementary 2). Aside from this, all interactions between participants and researchers minimized to not interfere with the participant’s thought processes [27, 31]. When analysis of the first case was complete, the researcher provided the second case, each lasting 35–45 min. A break between cases was offered. During and after interviews, field notes were recorded about initial impressions of the data collection session and potential patterns appearing to emerge [33].
Data analysis
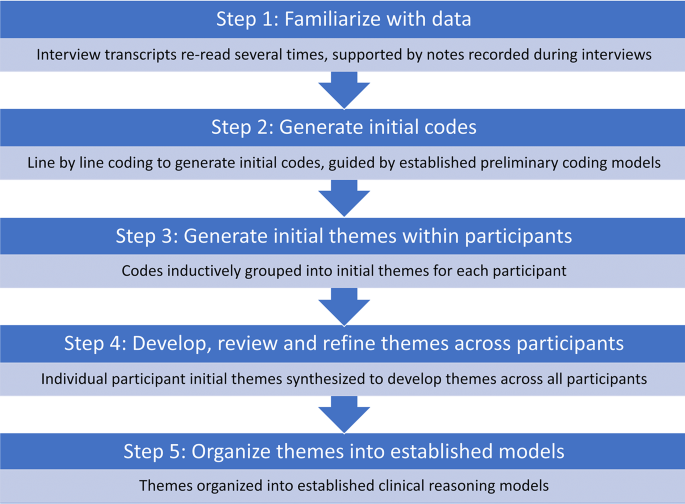
Data from think aloud interviews were analyzed using thematic analysis [30, 34], facilitating identification and analysis of patterns in data and key steps in the clinical reasoning process, including use of the Framework to enable its characterization (Fig. 1). As established models of clinical reasoning exist, a hybrid approach to thematic analysis was employed, incorporating inductive and deductive processes [35], which proceeded according to 5 iterative steps: [34]
-
1.
Familiarize with data: Audio-visual recordings were transcribed verbatim by a physiotherapist external to the research team. All transcripts were read and re-read several times by one researcher (KK), checking for accuracy by reviewing recordings as required. Field notes supported depth of familiarization with data.
-
2.
Generate initial codes: Line-by-line coding of transcripts by one researcher (KK) supported generation of initial codes that represented components, patterns and meaning in clinical reasoning processes and use of the Framework. Established preliminary coding models were used as a guide. Elstein’s diagnostic reasoning model [36] guided generating initial codes of key steps in clinical reasoning processes (Table 1a) [29, 36]. Leveraging richness of data, further codes were generated guided by the Postgraduate Musculoskeletal Physiotherapy Practice model, which describes masters level clinical practice (Table 1b) [12]. Codes were refined as data analysis proceeded. All codes were collated within participants along with supporting data.
-
3.
Generate initial themes within participants: Coded data was inductively grouped into initial themes within each participant, reflecting individual clinical reasoning processes and use of the Framework. This inductive stage enabled a systematic, flexible approach to describe each participant’s unique thinking path, offering insight into the complexities of their clinical reasoning processes. It also provided a comprehensive understanding of the Framework informing clinical reasoning and a rich characterization of its components, aiding the development of robust, nuanced insights [35, 37, 38]. Initial themes were repeatedly revised to ensure they were grounded in and reflected raw data.
-
4.
Develop, review and refine themes across participants: Initial themes were synthesized across participants to develop themes that represented all participants. Themes were reviewed and refined, returning to initial themes and codes at the individual participant level as needed.
-
5.
Organize themes into established models: Themes were deductively organized into established clinical reasoning models; first into Elstein’s diagnostic reasoning model, second into the Postgraduate Musculoskeletal Physiotherapy Practice model to characterize themes within each diagnostic reasoning component [12, 36].
Trustworthiness of findings
The research study was conducted according to an a priori protocol and additional steps were taken to establish trustworthiness of findings [39]. Field notes supported deep familiarization with data and served as a means of data source triangulation during analysis [40]. One researcher coded transcripts and a second researcher challenged codes, with codes and themes rigorously and iteratively reviewed and refined. Frequent debriefing sessions with the research team, reflexive discussions with other researchers and peer scrutiny of initial findings enabled wider perspectives and experiences to shape analysis and interpretation of findings. Several strategies were implemented to minimize the influence of prior relationships between participants and researchers, including author KK recruiting participants, KK and KH collecting/analyzing data, and AR, JS, HG and PP providing input on de-identified data at the stage of synthesis and interpretation.
Results
Participants
Nine AHCP postgraduate level students were recruited and participated in data collection. One participant was withdrawn because of unfamiliarity with the standardized teaching session about use of the Framework (no recall of session), despite confirmation of attendance. Data from eight participants were used for analysis (CMP: n = 6; SEM: n = 2; Table 2), which achieved sample size requirements for think aloud methodology of rich and in-depth data [27, 28].
Diagnostic reasoning components
Informed by the Framework, all components of Elstein’s diagnostic reasoning processes [36] were used by participants, including use of treatment with physiotherapy interventions to aid diagnostic reasoning. An illustrative example is presented in Supplement 3. Clinical reasoning used primarily hypothetico-deductive processes reflecting a continuum of proficiency, was informed by deep Framework knowledge and breadth of prior knowledge (e.g., experiential), and supported by a range of personal characteristics (e.g., justification for decisions).
Cue acquisition
All participants sought to acquire additional cues early in the patient history, and for some this persisted into the medical history and physical examination. Cue acquisition enabled depth and breadth of understanding patient history information to generate hypotheses and factors contributing to the patient’s pain experience (Table 3). All participants asked further questions to understand details of the patients’ pain and their presentation, while some also explored the impact of pain on patient functioning and treatments received to date. There was a high degree of specificity to questions for most participants. Ongoing clinical reasoning processes through a thorough and complete assessment, even if the patient had previously received treatment for similar symptoms, was important for some participants. Cue acquisition was supported by personal characteristics including a patient-centered approach (e.g., understanding the patient’s beliefs about pain) and one participant reflected on their approach to acquiring patient history cues.
Hypothesis generation
Participants generated an average of 4.5 hypotheses per case (range: 2–8) and most hypotheses (77%) were generated rapidly early in the patient history. Knowledge from the Framework about patient history features of vascular pathology informed vascular hypothesis generation in the patient history for all participants in both cases (Table 4). Vascular hypotheses were also generated during the past medical history, where risk factors for vascular pathology were identified and interpreted by some participants who had high levels of suspicion for cervical articular involvement. Non-vascular hypotheses were generated during the physical examination by some participants to explain individual physical examination or patient history cues. Deep knowledge of the patient history section in the Framework supported high level of cue identification and interpretation for generating vascular hypotheses. Initial hypotheses were prioritized by some participants, however the level of specificity of hypotheses varied.
Cue evaluation
All participants evaluated cues throughout the patient history and physical examination in relationship to hypotheses generated, indicating use of hypothetico-deductive reasoning processes (Table 5). Framework knowledge of patient history features of vascular pathology was used to test vascular hypotheses and aid differential diagnosis. The patient history section supported high level of cue identification and interpretation of patient history features for all but one participant, and generation of further patient history questions for all participants. The level of specificity of these questions was high for all but one participant. Framework knowledge of recommended physical examination tests, including removal of positional testing, supported planning a focused and prioritized physical examination to further test vascular hypotheses for all participants. No participant indicated intention to use positional testing as part of their physical examination. Treatment with physiotherapy interventions served as a form of cue evaluation, and cues were evaluated to inform prognosis for some participants. At times during the physical examination, some participants demonstrated occasional errors or difficulty with cue evaluation by omitting key physical exam tests (e.g., no cranial nerve assessment despite concerns for trigeminal nerve involvement), selecting physical exam tests in advance of hypothesis generation (e.g., cervical spine instability testing), difficulty interpreting cues, or late selection of a physical examination test. Cue acquisition was supported by a range of personal characteristics. Most participants justified selection of physical examination tests, and some self-reflected on their ability to collect useful physical examination information to inform selection of tests. Precaution to the physical examination was identified by all participants but one, which contributed to an adaptable approach, prioritizing patient safety and comfort. Critical analysis of physical examination information aided interpretation within the context of the patient for most participants.
Hypothesis evaluation
All participants used the Framework to evaluate their hypotheses throughout the patient history and physical examination, continuously shifting their level of support for hypotheses (Table 6, Supplement 4). This informed clarity in the overall level of suspicion for vascular pathology or musculoskeletal diagnoses, which were specific for most participants. Response to treatment with physiotherapy interventions served as a form of hypothesis evaluation for most participants who had low level suspicion for vascular pathology, highlighting ongoing reasoning processes. Hypotheses evaluated were prioritized by ranking according to level of suspicion by some participants. Difficulties weighing patient history and physical examination cues to inform judgement on overall level of suspicion for vascular pathology was demonstrated by some participants who reported that incomplete physical examination data and not being able to see the patient contributed to difficulties. Hypothesis evaluation was supported by the personal characteristic of reflection, where some students reflected on the Framework’s emphasis on the patient history to evaluate a vascular hypothesis.
Treatment
The Framework supported all participants in clinical reasoning related to treatment (Table 7). Treatment decisions were always linked to the participant’s overall level of suspicion for vascular pathology or musculoskeletal diagnosis. Framework knowledge supported participants with high level of suspicion for vascular pathology to refer for further investigations. Participants with a musculoskeletal diagnosis kept the patient for physiotherapy interventions. The Framework patient history section supported patient education about symptoms of vascular pathology and safety netting for some participants. Framework knowledge influenced informed consent processes and risk-benefit analysis to support the selection of musculoskeletal physiotherapy interventions, which were specific and prioritized for some participants. Less Framework knowledge related to treatment was demonstrated by some students, generating unclear recommendations regarding the urgency of referral and use of the Framework to inform musculoskeletal physiotherapy interventions. Treatment was supported by a range of personal characteristics. An adaptable approach that prioritized patient safety and was supported by justification was demonstrated in all participants except one. Shared decision-making enabled the selection of physiotherapy interventions, which were patient-centered (individualized, considered whole person, identified future risk for vascular pathology). Communication with the patient’s family doctor facilitated collaborative patient-centered care for most participants.
Discussion
This is the first study to explore the influence of the Framework on clinical reasoning processes in postgraduate physiotherapy students. The Framework supported clinical reasoning that used primarily hypothetico-deductive processes. The Framework informed vascular hypothesis generation in the patient history and testing the vascular hypothesis through patient history questions and selection of physical examination tests to inform clarity and support for diagnosis and management. Most postgraduate students’ clinical reasoning processes were characterized by high-level features (e.g. specificity, prioritization). However, some demonstrated occasional difficulties or errors, reflecting a continuum of clinical reasoning proficiency. Clinical reasoning processes were informed by deep knowledge of the Framework integrated with a breadth of wider knowledge and supported by a range of personal characteristics (e.g., justification for decisions, reflection).
Use of the Framework to inform clinical reasoning processes
The Framework provided a structured and comprehensive approach to support postgraduate students’ clinical reasoning processes in assessment and management of the cervical spine region, considering the potential for vascular pathology. Patient history and physical examination information was evaluated to inform clarity and support the decision to refer for further vascular investigations or proceed with musculoskeletal physiotherapy diagnosis/interventions. The Framework is not intended to lead to a vascular pathology diagnosis [7, 8], and following the Framework does not guarantee vascular pathologies will be identified [41]. Rather, it aims to support a process of clinical reasoning to elicit and interpret appropriate patient history and physical examination information to estimate the probability of vascular pathology and inform judgement about the need to refer for further investigations [7, 8, 42]. Results of this study suggest the Framework has achieved this aim for postgraduate physiotherapy students.
The Framework supported postgraduate students in using primarily hypothetico-deductive diagnostic reasoning processes. This is expected given the diversity of vascular pathology clinical presentations precluding a definite clinical pattern and inherent complexity as a potential masquerader of a musculoskeletal problem [7]. It is also consistent with prior research investigating clinical reasoning processes in musculoskeletal physiotherapy postgraduate students [12] and clinical experts [29] where hypothetico-deductive and pattern recognition diagnostic reasoning are employed according to the demands of the clinical situation [10]. Diagnostic reasoning of most postgraduate students in this study demonstrated features suggestive of high-level clinical reasoning in musculoskeletal physiotherapy [12], including ongoing reasoning with high-level cue identification and interpretation, specificity and prioritization during assessment and treatment, use of physiotherapy interventions to aid diagnostic reasoning, and prognosis determination [12, 29, 43]. Expert physiotherapy practice has been further described as using a dialectical model of clinical reasoning with seamless transitions between clinical reasoning strategies [44]. While diagnostic reasoning was a focus in this study, postgraduate students considered a breadth of information as important to their reasoning (e.g., patient’s perspectives of the reason for their pain). This suggests wider reasoning strategies (e.g., narrative, collaborative) were employed to enable shared decision-making within the context of patient-centered care.
Study findings also highlighted a continuum of proficiency in use of the Framework to inform clinical reasoning processes. Not all students demonstrated all characteristics of high-level clinical reasoning and there are suggestions of incomplete reasoning processes, for example occasional errors in evaluating cues. Some students offered explanations such as incomplete case information as factors contributing to difficulties with clinical reasoning processes. However, the ability to critically evaluate incomplete and potentially conflicting clinical information is consistently identified as an advanced clinical practice competency [14, 43]. A continuum of proficiency in clinical reasoning in musculoskeletal physiotherapy is supported by wider healthcare professions describing acquisition and application of clinical knowledge and skills as a developmental continuum of clinical competence progressing from novice to expert [45, 46]. The range of years of clinical practice experience in this cohort of students (3–14 years) or prior completed postgraduate education may have contributed to the continuum of proficiency, as high-quality and diverse experiential learning is essential for the development of high-level clinical reasoning [14, 47].
Deep knowledge of the Framework informs clinical reasoning processes
Postgraduate students demonstrated deep Framework knowledge to inform clinical reasoning processes. All students demonstrated knowledge of patient history features of vascular pathology, recommended physical examination tests to test a vascular hypothesis, and the need to refer if there is a high level of suspicion for vascular pathology. A key development in the recent Framework update is the removal of the recommendation to perform positional testing [8]. All students demonstrated knowledge of this development, and none wanted to test a vascular hypothesis with positional testing. Most also demonstrated Framework knowledge about considerations for planning treatment with physiotherapy interventions (e.g., risk-benefit analysis, informed consent), though not all, which underscores the continuum of proficiency in postgraduate students. Rich organization of multidimensional knowledge is a required component for high level clinical reasoning and is characteristic of expert physiotherapy practice [10, 48, 49]. Most postgraduate physiotherapy students displayed this expert practice characteristic through integration of deep Framework knowledge with a breadth of prior knowledge (e.g., experiential, propositional) to inform clinical reasoning processes. This highlights the utility of the Framework in postgraduate physiotherapy education to develop advanced level evidence-based knowledge informing clinical reasoning processes for safe assessment and management of the cervical spine, considering the potential for vascular pathology [9, 8, 50,51,52].
Framework supports personal characteristics to facilitate integration of knowledge and clinical reasoning
The Framework supported personal characteristics of postgraduate students, which are key drivers for the complex integration of advanced knowledge and high-level clinical reasoning [10, 12, 48]. For all students, the Framework supported justification for decisions and patient-centered care, emphasizing a whole-person approach and shared decision-making. Further demonstrating a continuum of proficiency, the Framework supported a wider breadth of personal characteristics for some students, including critical analysis, reflection, self-analysis, and adaptability. These personal characteristics illustrate the interwoven cognitive and metacognitive skills that influence and support a high level of clinical reasoning [10, 12] and the development of clinical expertise [48, 53]. For example [54], reflection is critical to developing high-level clinical reasoning and advanced level practice [12, 55]. Postgraduate students reflected on prior knowledge, experiences, and action within the context of current Framework knowledge, emphasizing active engagement in cognitive processes to inform clinical reasoning processes. Reflection-in-action is highlighted by self-analysis and adaptability. These characteristics require continuous cognitive processing to consider personal strengths and limitations in the context of the patient and evidence-based practice, adapting the clinical encounter as required [53, 55]. These findings highlight use of the Framework in postgraduate education to support development of personal characteristics that are indicative of an advanced level of clinical practice [12].
Synthesis of findings
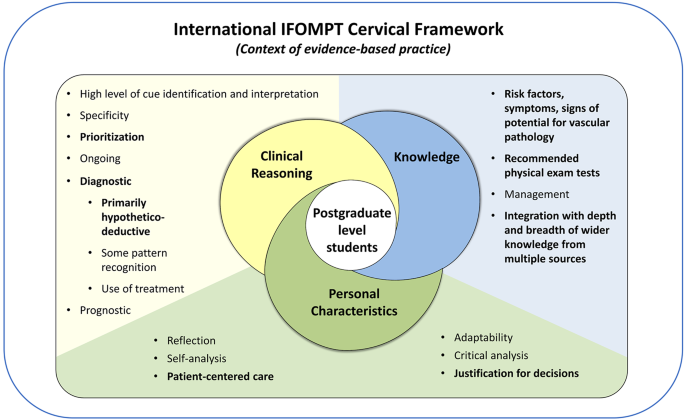
Derived from synthesis of research study findings and informed by the Postgraduate Musculoskeletal Physiotherapy Practice model [12], use of the Framework to inform clinical reasoning processes in postgraduate students is illustrated in Fig. 2. Overlapping clinical reasoning, knowledge and personal characteristic components emphasize the complex interaction of factors contributing to clinical reasoning processes. Personal characteristics of postgraduate students underpin clinical reasoning and knowledge, highlighting their role in facilitating the integration of these two components. Bolded subcomponents indicate convergence of results reflecting all postgraduate students and underscores the variability among postgraduate students contributing to a continuum of clinical reasoning proficiency. The relative weighting of the components is approximately equal to balance the breadth and convergence of subcomponents. Synthesis of findings align with the Postgraduate Musculoskeletal Physiotherapy Practice model [12], though some differences exist. Limited personal characteristics were identified in this study with little convergence across students, which may be due to the objective of this study and the case analysis approach.
Use of the Framework to inform clinical reasoning in postgraduate level musculoskeletal physiotherapy students. Adapted from the Postgraduate Musculoskeletal Physiotherapy Practice model [12].
Strengths and limitations
Think aloud case analyses enabled situationally dependent understanding of the Framework to inform clinical reasoning processes in postgraduate level students [17], considering the rare potential for vascular pathology. A limitation of this approach was the standardized nature of case information provided to students, which may have influenced clinical reasoning processes. Future research studies may consider patient case simulation to address this limitation [30]. Interviews were conducted during the second half of the postgraduate educational program, and this timing could have influenced clinical reasoning processes compared to if interviews were conducted at the end of the program. Future research can explore use of the Framework to inform clinical reasoning processes in established advanced practice physiotherapists. The sample size of this study aligns with recommendations for think aloud methodology [27, 28], achieved rich data, and purposive sampling enabled wide representation of key characteristics (e.g., gender, ethnicity, country of training, physiotherapy experiences), which enhances transferability of findings. Students were aware of the study objective in advance of interviews which may have contributed to a heightened level of awareness of vascular pathology. The prior relationship between students and researchers may have also influenced results, however several strategies were implemented to minimize this influence.
Implications
The Framework is widely implemented within IFOMPT postgraduate educational programs and has led to important shifts in educational curricula [9]. Findings of this study support use of the Framework as an educational resource in postgraduate physiotherapy programs to inform clinical reasoning processes for safe and effective assessment and management of cervical spine presentations considering the potential for vascular pathology. Individualized approaches may be required to support each student, owing to a continuum of clinical reasoning proficiency. As the Framework was written for practicing musculoskeletal clinicians, future research is required to explore use of the Framework to inform clinical reasoning in learners at different levels, for example entry-level physiotherapy students.
Conclusions
The Framework supported clinical reasoning that used primarily hypothetico-deductive processes in postgraduate physiotherapy students. It informed vascular hypothesis generation in the patient history and testing the vascular hypothesis through patient history questions and selection of physical examination tests, to inform clarity and support for diagnosis and management. Most postgraduate students clinical reasoning processes were characterized as high-level, informed by deep Framework knowledge integrated with a breadth of wider knowledge, and supported by a range of personal characteristics to facilitate the integration of advanced knowledge and high-level clinical reasoning. Future research is required to explore use of the Framework to inform clinical reasoning in learners at different levels.
Data availability
The dataset used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Safiri S, Kolahi AA, Hoy D, Buchbinder R, Mansournia MA, Bettampadi D et al. Global, regional, and national burden of neck pain in the general population, 1990–2017: systematic analysis of the global burden of Disease Study 2017. BMJ. 2020;368.
Stovner LJ, Nichols E, Steiner TJ, Abd-Allah F, Abdelalim A, Al-Raddadi RM, et al. Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the global burden of Disease Study 2016. Lancet Neurol. 2018;17:954–76.
Cieza A, Causey K, Kamenov K, Hanson SW, Chatterji S, Vos T. Global estimates of the need for rehabilitation based on the Global Burden of Disease study 2019: a systematic analysis for the global burden of Disease Study 2019. Lancet. 2020;396:2006–17.
Côté P, Yu H, Shearer HM, Randhawa K, Wong JJ, Mior S et al. Non-pharmacological management of persistent headaches associated with neck pain: A clinical practice guideline from the Ontario protocol for traffic injury management (OPTIMa) collaboration. European Journal of Pain (United Kingdom). 2019;23.
Diamanti S, Longoni M, Agostoni EC. Leading symptoms in cerebrovascular diseases: what about headache? Neurological Sciences. 2019.
Debette S, Compter A, Labeyrie MA, Uyttenboogaart M, Metso TM, Majersik JJ, et al. Epidemiology, pathophysiology, diagnosis, and management of intracranial artery dissection. Lancet Neurol. 2015;14:640–54.
Rushton A, Carlesso LC, Flynn T, Hing WA, Rubinstein SM, Vogel S, et al. International Framework for examination of the Cervical Region for potential of vascular pathologies of the Neck Prior to Musculoskeletal intervention: International IFOMPT Cervical Framework. J Orthop Sports Phys Therapy. 2023;53:7–22.
Rushton A, Carlesso LC, Flynn T, Hing WA, Kerry R, Rubinstein SM, et al. International framework for examination of the cervical region for potential of vascular pathologies of the neck prior to orthopaedic manual therapy (OMT) intervention: International IFOMPT Cervical Framework. International IFOMPT Cervical Framework; 2020.
Hutting N, Kranenburg R, Taylor A, Wilbrink W, Kerry R, Mourad F. Implementation of the International IFOMPT Cervical Framework: a survey among educational programmes. Musculoskelet Sci Pract. 2022;62:102619.
Jones MA, Jensen G, Edwards I. Clinical reasoning in physiotherapy. In: Campbell S, Watkins V, editors. Clinical reasoning in the health professions. Third. Philadelphia: Elsevier; 2008. pp. 245–56.
Fennelly O, Desmeules F, O’Sullivan C, Heneghan NR, Cunningham C. Advanced musculoskeletal physiotherapy practice: informing education curricula. Musculoskelet Sci Pract. 2020;48:102174.
Rushton A, Lindsay G. Defining the construct of masters level clinical practice in manipulative physiotherapy. Man Ther. 2010;15.
Rushton A, Lindsay G. Defining the construct of masters level clinical practice in healthcare based on the UK experience. Med Teach. 2008;30:e100–7.
Noblet T, Heneghan NR, Hindle J, Rushton A. Accreditation of advanced clinical practice of musculoskeletal physiotherapy in England: a qualitative two-phase study to inform implementation. Physiotherapy (United Kingdom). 2021;113.
Tawiah AK, Stokes E, Wieler M, Desmeules F, Finucane L, Lewis J, et al. Developing an international competency and capability framework for advanced practice physiotherapy: a scoping review with narrative synthesis. Physiotherapy. 2023;122:3–16.
Williams A, Rushton A, Lewis JJ, Phillips C. Evaluation of the clinical effectiveness of a work-based mentoring programme to develop clinical reasoning on patient outcome: a stepped wedge cluster randomised controlled trial. PLoS ONE. 2019;14.
Miles R. Complexity, representation and practice: case study as method and methodology. Issues Educational Res. 2015;25.
Thorne S, Kirkham SR, MacDonald-Emes J. Interpretive description: a noncategorical qualitative alternative for developing nursing knowledge. Res Nurs Health. 1997;20.
Thorne S, Kirkham SR, O’Flynn-Magee K. The Analytic challenge in interpretive description. Int J Qual Methods. 2004;3.
Creswell JW. Research design: qualitative, quantitative, and mixed methods approaches. Sage; 2003.
Dolan S, Nowell L, Moules NJ. Interpretive description in applied mixed methods research: exploring issues of fit, purpose, process, context, and design. Nurs Inq. 2023;30.
Thorne S. Interpretive description. In: Routledge International Handbook of Qualitative Nursing Research. 2013. pp. 295–306.
Thompson Burdine J, Thorne S, Sandhu G. Interpretive description: a flexible qualitative methodology for medical education research. Med Educ. 2021;55.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus group. Int J Qual Health Care. 2007;19:349–57.
Archibald MM, Ambagtsheer RC, Casey MG, Lawless M. Using zoom videoconferencing for qualitative data Collection: perceptions and experiences of researchers and participants. Int J Qual Methods. 2019;18.
Van Someren M, Barnard YF, Sandberg J. The think aloud method: a practical approach to modelling cognitive. Volume 11. London: Academic; 1994.
Fonteyn ME, Kuipers B, Grobe SJ. A description of think aloud Method and Protocol Analysis. Qual Health Res. 1993;3:430–41.
Lundgrén-Laine H, Salanterä S. Think-Aloud technique and protocol analysis in clinical decision-making research. Qual Health Res. 2010;20:565–75.
Doody C, McAteer M. Clinical reasoning of expert and novice physiotherapists in an outpatient orthopaedic setting. Physiotherapy. 2002;88.
Gilliland S. Physical therapist students’ development of diagnostic reasoning: a longitudinal study. J Phys Therapy Educ. 2017;31.
Ericsson KA, Simon HA. How to study thinking in Everyday Life: contrasting think-aloud protocols with descriptions and explanations of thinking. Mind Cult Act. 1998;5:178–86.
Dwyer SC, Buckle JL. The space between: on being an insider-outsider in qualitative research. Int J Qual Methods. 2009;8.
Shenton AK. Strategies for ensuring trustworthiness in qualitative research projects. Educ Inform. 2004;22:63–75.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101.
Fereday J, Muir-Cochrane E. Demonstrating Rigor using thematic analysis: a Hybrid Approach of Inductive and deductive coding and theme development. Int J Qual Methods. 2006;5.
Elstein ASLSS. Medical problem solving: an analysis of clinical reasoning. Harvard University Press; 1978.
Proudfoot K. Inductive/Deductive Hybrid Thematic Analysis in mixed methods research. J Mix Methods Res. 2023;17.
Charters E. The use of think-aloud methods in qualitative research an introduction to think-aloud methods. Brock Educ J. 2003;12.
Nowell LS, Norris JM, White DE, Moules NJ. Thematic analysis: striving to meet the trustworthiness Criteria. Int J Qual Methods. 2017;16:1–13.
Thurmond VA. The point of triangulation. J Nurs Scholarsh. 2001;33.
Hutting N, Wilbrink W, Taylor A, Kerry R. Identifying vascular pathologies or flow limitations: important aspects in the clinical reasoning process. Musculoskelet Sci Pract. 2021;53:102343.
de Best RF, Coppieters MW, van Trijffel E, Compter A, Uyttenboogaart M, Bot JC, et al. Risk assessment of vascular complications following manual therapy and exercise for the cervical region: diagnostic accuracy of the International Federation of Orthopaedic Manipulative physical therapists framework (the Go4Safe project). J Physiother. 2023;69:260–6.
Petty NJ. Becoming an expert: a masterclass in developing clinical expertise. Int J Osteopath Med. 2015;18:207–18.
Edwards I, Jones M, Carr J, Braunack-Mayer A, Jensen GM. Clinical reasoning strategies in physical therapy. Phys Ther. 2004;84.
Carraccio CL, Benson BJ, Nixon LJ, Derstine PL. Clinical teaching from the Educational Bench to the clinical Bedside: Translating the Dreyfus Developmental Model to the Learning of Clinical Skills.
Benner P. Using the Dreyfus Model of Skill Acquisition to describe and interpret Skill Acquisition and Clinical Judgment in nursing practice and education. Bull Sci Technol Soc. 2004;24:188–99.
Benner P. From novice to expert: Excellence and power in clinical nursing practice. Upper Saddle River, New Jersey: Prentice Hall;: Commemorative Ed; 2001.
Jensen GM, Gwyer J, Shepard KF, Hack LM. Expert practice in physical therapy. Phys Ther. 2000;80.
Huhn K, Gilliland SJ, Black LL, Wainwright SF, Christensen N. Clinical reasoning in physical therapy: a Concept Analysis. Phys Ther. 2019;99.
Hutting N, Kranenburg HA, Rik KR. Yes, we should abandon pre-treatment positional testing of the cervical spine. Musculoskelet Sci Pract. 2020;49:102181.
Kranenburg HA, Tyer R, Schmitt M, Luijckx GJ, Schans C, Van Der, Hutting N, et al. Effects of head and neck positions on blood flow in the vertebral, internal carotid, and intracranial arteries: a systematic review. J Orthop Sports Phys Ther. 2019;49:688–97.
Hutting N, Kerry R, Coppieters MW, Scholten-Peeters GGM. Considerations to improve the safety of cervical spine manual therapy. Musculoskelet Sci Pract. 2018;33.
Wainwright SF, Shepard KF, Harman LB, Stephens J. Novice and experienced physical therapist clinicians: a comparison of how reflection is used to inform the clinical decision-making process. Phys Ther. 2010;90:75–88.
Dy SM, Purnell TS. Key concepts relevant to quality of complex and shared decision-making in health care: a literature review. Soc Sci Med. 2012;74:582–7.
Christensen N, Jones MA, Higgs J, Edwards I. Dimensions of clinical reasoning capability. In: Campbell S, Watkins V, editors. Clinical reasoning in the health professions. 3rd edition. Philadelphia: Elsevier; 2008. pp. 101–10.
Acknowledgements
The authors would like to acknowledge study participants and the transcriptionist for their time in completing and transcribing think aloud interviews.
Funding
No funding was received to conduct this research study.
Author information
Authors and Affiliations
Contributions
Katie Kowalski: Conceptualization, methodology, validation, formal analysis, investigation, data curation, writing– original draft, visualization, project administration. Heather Gillis: Validation, resources, writing– review & editing. Katherine Henning: Investigation, formal analysis, writing– review & editing. Paul Parikh: Validation, resources, writing– review & editing. Jackie Sadi: Validation, resources, writing– review & editing. Alison Rushton: Conceptualization, methodology, validation, writing– review & editing, supervision.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Western University Health Science Research Ethics Board granted ethical approval (Project ID: 119934). Participants provided written informed consent prior to participating in think aloud interviews.
Consent for publication
Not applicable.
Competing interests
Author AR is an author of the IFOMPT Cervical Framework. Authors JS and HG are lecturers on the AHCP CMP program. AR and JS led standardized teaching of the Framework. Measures to reduce the influence of potential competing interests on the conduct and results of this study included: the Framework representing international and multiprofessional consensus, recruitment of participants by author KK, data collection and analysis completed by KK with input from AR, JS and HG at the stage of data synthesis and interpretation, and wider peer scrutiny of initial findings. KK, KH and PP have no potential competing interests.
Authors’ information
The lead author of this study (AR) is the first author of the International IFOMPT Cervical Framework.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kowalski, K.L., Gillis, H., Henning, K. et al. Use of the International IFOMPT Cervical Framework to inform clinical reasoning in postgraduate level physiotherapy students: a qualitative study using think aloud methodology. BMC Med Educ 24, 486 (2024). https://0-doi-org.brum.beds.ac.uk/10.1186/s12909-024-05399-x
Received:
Accepted:
Published:
DOI: https://0-doi-org.brum.beds.ac.uk/10.1186/s12909-024-05399-x