- Research
- Open access
- Published:
Perception, practice, and barriers toward research among pediatric undergraduates: a cross-sectional questionnaire-based survey
BMC Medical Education volume 24, Article number: 364 (2024)
Abstract
Background
Scientific research activities are crucial for the development of clinician-scientists. However, few people pay attention to the current situation of medical research in pediatric medical students in China. This study aims to assess the perceptions, practices and barriers toward medical research of pediatric undergraduates.
Methods
This cross-sectional study was conducted among third-year, fourth-year and fifth-year pediatric students from Zhejiang University School of Medicine in China via an anonymous online questionnaire. The questionnaires were also received from fifth-year students majoring in other medicine programs [clinical medicine (“5 + 3”) and clinical medicine (5-year)].
Results
The response rate of pediatric undergraduates was 88.3% (68/77). The total sample of students enrolled in the study was 124, including 36 students majoring in clinical medicine (“5 + 3”) and 20 students majoring in clinical medicine (5-year). Most students from pediatrics (“5 + 3”) recognized that research was important. Practices in scientific research activities are not satisfactory. A total of 51.5%, 35.3% and 36.8% of the pediatric students participated in research training, research projects and scientific article writing, respectively. Only 4.4% of the pediatric students contributed to publishing a scientific article, and 14.7% had attended medical congresses. None of them had given a presentation at a congress. When compared with fifth-year students in the other medicine program, the frequency of practices toward research projects and training was lower in the pediatric fifth-year students. Lack of time, lack of guidance and lack of training were perceived as the main barriers to scientific work. Limited English was another obvious barrier for pediatric undergraduates. Pediatric undergraduates preferred to participate in clinical research (80.9%) rather than basic research.
Conclusions
Although pediatric undergraduates recognized the importance of medical research, interest and practices in research still require improvement. Lack of time, lack of guidance, lack of training and limited English were the common barriers to scientific work. Therefore, research training and English improvement were recommended for pediatric undergraduates.
Background
Medical education includes the learning of basic clinical medical knowledge and the cultivation of scientific research abilities. Scientific research, an essential part of medical education, is increasingly important, as it can greatly improve medical care [1, 2]. Scientific research activities are crucial for the development of clinician-scientists, who have key roles in clinical research and translational medicine. Therefore, medical education is increasingly emphasizing the cultivation of scientific research abilities. Strengthening scientific research training helps students to develop independent critical thinking, improve the ability of observation, and foster the problem-solving skills. It is suggested that developing undergraduate research benefits the students, the faculty mentors, the university or institution, and eventually society [2, 3]. As a result, there is a growing trend to integrate scientific research training into undergraduate medical education. Early exposure to scientific research was recommended in undergraduate medical students [4, 5]. In fact, an international questionnaire study showed that among 1625 responses collected from 38 countries, less than half (42.7%) agree/strongly agree that their medical schools provided “sufficient training in medical research” [6]. The training or practices about medical research in undergraduates is not universal. In China, few people pay attention to the current situation of medical research in undergraduates, especially for pediatric medical students.
Due to changes in China’s birth policy (two-child policy in 2016 and the three-child policy in 2021), child health needs are increasing [7]. The shortage of pediatricians is alarming in China. Therefore, numerous policies have been implemented to meet the challenges of the shortage of pediatricians, including reinstating pediatrics as an independent discipline in medical school enrollment and increasing the enrollment of pediatrics. The number of pediatricians has increased year by year. The number of pediatricians in China increased from 118,500 in 2015 (0.52 pediatricians per 1000 children under the age of 14) to 206,000 in 2021 (0.78 pediatricians per 1000 children under the age of 14). With the increase in pediatric enrollment, pediatric medical education is facing new challenges. It is urgent to study the current situation of cultivation of pediatric medical students, one of which is the scientific research abilities [8, 9]. However, as the particular background of pediatrics, very little is known about the perception, practice and barriers toward medical research in pediatric undergraduates. The purpose of this study was to address the gap by assessing the practices, perceptions and barriers toward medical research of pediatric undergraduates at Zhejiang University. The results can help to improve the mode of cultivating scientific research abilities among pediatric medical students.
Methods
The study was conducted from March to April 2023. The study was approved by the Ethics Review Committee of the Children’s Hospital of Zhejiang University School of Medicine and was undertaken according to the Helsinki declaration. Participants provided written informed consent upon applying to participate in the study.
Study design and setting
This is a cross-sectional study conducted via an online questionnaire and the questionnaire was done simultaneously in all students. The study aimed to investigate the perception, practices and barriers toward research in pediatric undergraduates from Zhejiang University School of Medicine, and to investigate the differences in research among undergraduate students from clinical medicine (“5 + 3” integrated program, pediatrics) [pediatrics (“5 + 3”)], clinical medicine (“5 + 3” integrated program) [clinical medicine (“5 + 3”)] and clinical medicine (5-year).
The clinical medicine of Zhejiang University School of Medicine (ZUSM) includes a 5-year program, a “5 + 3” integrated program, and a 8-year MD. Program. The clinical medicine (5-year) program is the basis of clinical medicine education.Graduates need to complete 3 years of standardized residency training to become doctors. The clinical medicine (“5 + 3”) model combines the 5-year medical undergraduate education, 3-year standardized residency training and postgraduate education. Since 2015, 20 to 30 students who are interested in pediatrics were selected from second-year undergraduate students of clinical medicine (“5 + 3”) to continue studies as pediatrics (“5 + 3”) every year. Since 2019, ZUSM established pediatrics (“5 + 3”) program. 20–30 students have been enrolled independently every year.
Participants
All of the third-, fourth-, and fifth-year undergraduate students in pediatrics (“5 + 3”) and some of the fifth-year undergraduate students from clinical medicine (“5 + 3”) and clinical medicine (5-year) who expressed an interest in participating in the study were enrolled.
Data collection
The questionnaire was self-designed after reviewing the literature and consulting senior faculty. For the purpose of testing its clarity and reliability, the questionnaire was pilot tested among 36 undergraduate students. Their feedback was mainly related to the structure of the questionnaire. To address these comments, the questionnaire was modified to reach the final draft, which was distributed to the student sample included in the study. The reliability coefficient was assessed by Cronbach’s alpha, and the validity was evaluated by Kaiser-Meyer-Olkin (KMO).
There are four sections of the questionnaire used in this study:
The first part covered 3 statements (gender, grade and major).
The second part examined the participants’ perceptions of medical research, including 5 statements (importance, enhancement of competitiveness, practising thinking ability, solving clinical problems, and being interesting).
The third part examined practices in medical research, including 6 statements (project, training, write paper, publish paper, attend academic conference and conference communication).
The barriers to medical research were assessed in the last part, including 7 statements.
Perception and barriers toward medical research were evaluated using a five-point Likert scale ranging from 1 to 5 (1 = strongly disagree; 2 = disagree, 3 = uncertain, 4 = agree, 5 = strongly agree).
Statistical analysis
Categorical data are represented as numbers and frequencies. For ease of reporting and analyzing data, the responses of “agree” and “strongly agree” were grouped and reported as agreements, and “disagree” and “strongly disagree” were grouped as disagreements. The chi-square test was used to test the difference in the frequency of participation in research practices. The student’s perception score based on grades was analyzed using Fisher’s exact test, and attitude between the year of study was analyzed by ANOVA or a nonparametric test (Kruskal-Wallis H test). The statistical analysis was performed using IBM SPSS version 26. P < 0.05 was considered significant.
Results
The reliability coefficient of the questionnaire was assessed by Cronbach’s alpha; it was 0.73 for perception and 0.78 for barriers. KMO was 0.80 for perception (Bartlett’s sphericity test: χ2 = 200.4, p < 0.001) and 0.73 for barriers (Bartlett’s sphericity test: χ2 = 278.4, p < 0.001), indicating the appropriateness of the factor analysis. The factor analysis was carried out using the principal component analysis with varimax rotation. For perception, one factor explains 58.2% of the variance. For barriers, two-factor solution explains 60.2% of the variance.
The response rate was 79.2% (19/24) in the third year, 88% (22/25) in the fourth year and 96.4% (27/28) in the fifth year students in pediatrics (“5 + 3”), and the total response rate was 88.3% (68/77). The number of fifth-year students majoring in clinical medicine (“5 + 3”) and clinical medicine (5-year) was 36 and 20, respectively. Thus, a total of 124 students participated in the questionnaire. Among the participants, approximately 46% were male and 54% were female.
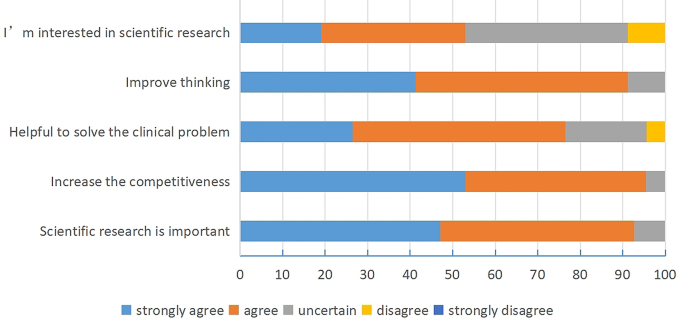
Perception regarding scientific research among the students majoring in pediatrics (“5 + 3”)
The majority of students in pediatrics (“5 + 3”) recognized that research was important (92.6%), such as increasing competitiveness, solving clinical problems and improving thinking (Fig. 1). Approximately half of the students in pediatrics (“5 + 3”) were interested in the research.
Among the third-, fourth-, and fifth-year students in pediatrics (“5 + 3”), there was a significant difference in the effect of research on thinking ability (Table 1). A stronger understanding of the importance of research for thinking abilities was found in students from the fifth year.
Comparing the perception of medical research among the fifth-year students from the different medicine programs, there was a significant difference in the interest in research (Table 2). The fifth-year undergraduates from clinical medicine (5-year) received the highest score for interest in scientific research, followed by pediatrics (“5 + 3”).
Practices regarding scientific research among students majoring in pediatrics (“5 + 3”)
More than half of the students in pediatrics (“5 + 3”) participated in research training. Approximately 36.8% of them were involved in writing scientific articles, and 35.3% participated in research projects (Table 3). Only 4.4% of the students in pediatrics (“5 + 3”) contributed to publishing a scientific article, and 14.7% of the students in pediatrics (“5 + 3”) had attended medical congresses. However, none of the students had made a presentation at congresses.
A statistically significant difference was observed among different grades in the pediatrics (“5 + 3”) program, with fifth-year students having a much higher rate of participation in conferences. However, no significant differences were observed in other forms of medical research practices.
When compared with fifth-year students from other programs (clinical medicine “5 + 3” or 5-year), the students in pediatrics (“5 + 3”) had a lower rate of participation in the projects (Table 4). The rate of participation in the research training of the pediatric students was lower than that of clinical medicine (5-year) (44.44% vs. 75%). There were no significant differences in other research practices, such as writing articles and attending congress.
Barriers regarding scientific research among the students majoring in pediatrics (“5 + 3”)
The most common barriers to research work for pediatric students were lack of training (85.3%), lack of time (83.9%), and lack of mentorship (82.4%).
However, the top three barriers to research work in fifth-year pediatric students were lack of training (96.3%), limited English (88.89%) and lack of time (88.89%). We found that the barrier of “lack of training” became increasingly apparent with grade, which was significantly obvious in fifth-year pediatric students compared with other grades (Table 5). The other barriers had no significant differences among the three grades from the pediatrics (“5 + 3”) program.
When compared with fifth-year students from other programs (clinical medicine “5 + 3” or 5-year), the rate of agreement about the barrier of “limited English” was significantly higher in fifth-year students from the pediatrics (“5 + 3”) program. There were no significant differences in other barriers among fifth-year students from different majors (Table 6).
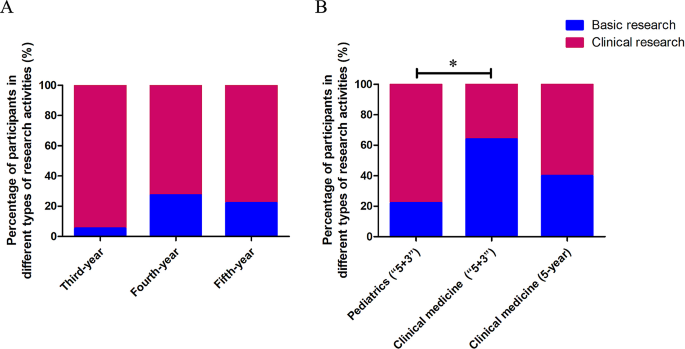
The type of research activities willing to involve in the future among the students majoring in pediatrics (“5 + 3”)
A total of 88.2% of students in pediatrics (“5 + 3”) wanted to participate in the training of scientific research activities. Furthermore, when asked about the type of future scientific research activities, 80.9% of students wanted to participate in clinical research, and only 19.1% of students wanted to be involved in basic research. There was no significant difference in the different grades of the students from the pediatrics (“5 + 3”) program (Fig. 2A).
Types of research activities that students majoring in pediatrics are willing to be involved with in the future (A). Types of research activities that the students from different programs are willing to be involved with in the future (B). When compared with students in clinical medicine (“5 + 3”), fifth-year students in pediatrics (“5 + 3”) were significantly less likely to participate in basic research (*P = 0.001)
Compared with students in clinical medicine (“5 + 3”), fifth-year students in pediatrics (“5 + 3”) were significantly less likely to participate in basic research (Fig. 2B).
Discussion
In China, to solve the shortage of pediatricians, pediatric programs have resumed in some medical schools, including Zhejiang University, in recent years. In this study, we focused on the perceptions, practices and barriers to scientific research in pediatric undergraduates from Zhejiang University.
With global progress, more research is required to advance knowledge and innovation in all fields. Likewise, at the present time, research activities are a highly important skill for medical practitioner. Medical students were encouraged to take active part in scientific research and prepare for today’s knowledge-driven world [2]. In the current study, we found an overall positive perception of scientific research in pediatric undergraduates. More than 90% of pediatric students agreed (“strongly agree” and “agree”) that scientific research was important, which could make them more competitive and improve their thinking.
Although the students had a positive perception of medical research, their practice of conducting research remained unsatisfactory. When compared with the fifth-year undergraduates from clinical medicine (“5 + 3”) (66.67%) and clinical medicine (5-year) (75%), only 33.33% of the fifth-year undergraduates in pediatrics (“5 + 3”) have participated in scientific research projects. The number of paper publications was very small (third-year of Pediatric (“5 + 3”) 0, fourth-year 4.5% and fifth-year 7.4%). It was significantly less than the publication rate of final-year students in the United States (46.5%) and Australia (roughly one-third) [10, 11]. In another study in Romania, 31% of fifth-year students declared that they had prepared a scientific presentation for a medical congress at least once [12]. Moreover, none of the students in the study presented their paper in the scientific forum. A study in India also found that the undergraduate students’ experience of presenting paper in scientific forums was only 5% and publication 5.6% [13]. As part of the curriculum, some Indian universities require postgraduates to present papers and submit manuscripts for publication. Nevertheless, the practices regarding scientific research of undergraduates is still relatively poor. Lack of time, lack of guidance and lack of training for research careers were found to be the major obstacles in medical research for both pediatric students and others, which is consistent with previous reports [5, 14, 15]. The questionnaire in residents also found that lack of time was a critical problem for scientific research [16]. There is no common practice about how to solve this difficulty. In the literature, it was usually recommended that integration of scientific research training into the curricular requirements for undergraduates or residency programs for residents should be implemented [7, 14, 17, 18]. An increasing number of medical schools have individual projects as a component of their curriculum or mandatory medical research projects to develop research competencies [19, 20].
Interestingly, in fifth-year pediatric undergraduates (“5 + 3”), English limitations were found to be one of the most common barriers. The barrier of the limitation of English was increasingly better as the grades increased in pediatric students. We speculated that this was related to the increasing awareness of the importance of scientific research and participation in scientific research activities, increasing demand for reading English literature and writing English articles. Furthermore, the English limitation barrier for pediatric students was more obvious than that for students from clinical medicine (“5 + 3”) and clinical medicine (5-year). They are worried about academic English. Horwitz et al. first proposed “foreign language anxiety” [21]. Deng and Zhou explored medical students’ medical English anxiety in Sichuan, China. They found that 85.2% of the students surveyed suffered moderate above medical English anxiety [22]. In the questionnaire, 88.89% of the fifth-year pediatric students believed that limited English was one of the most important barriers for scientific research. Currently, English is the chief language of communication in the field of medical science, including correspondence, conferences, writing scientific articles, and reading literature. Ma Y noted that medical English should be the most important component of college English teaching for medical students [23]. At Zhejiang University, all of the students, including those majoring in pediatrics (“5 + 3”), clinical medicine (“5 + 3”) and clinical medicine (5-year), had a medical English course during the undergraduate period. Thus, the course could not satisfy the demands for scientific research, such as reading English literature, writing English paper and oral presentation in English. To solve this barrier, it was suggested to understand the requirements of pediatric students for medical English learning and offer more courses about medical English or English writing training for pediatric students. Furthermore, undergraduates should be encouraged to participate in local, regional or national conferences that are not in English but in Chinese language, which can increase the interest in participating in scientific research.
Most of the pediatric students tended to choose clinical research, while only 19.1% wanted to attend basic research. The proportion of fifth-year students in pediatrics (“5 + 3”) choosing basic research was much lower than the students from the clinical medicine (“5 + 3”) program. It is speculated that pediatrics usually have heavier clinical work with relative poor scientific practice in China, compare with doctors from other clinical department. They are likely to concern the clinical research. The students in pediatrics might not obtain sufficient scientific guidance from their clinician teachers compared with those from other medicine program. According to the data, the Pediatric College could conduct more scientific research training directed at clinical research, such as the design, conduct and administration of clinical trials. The simulation-based clinical research curriculum is considered to be a better approach training of clinician-scientists compared with traditional clinical research teaching [24]. On the other hand, we might need to do more to improve the interest in basic research for pediatric undergraduates.
The major limitation of the present study is the small sample size. Only 20 to 30 students have been enrolled in pediatrics (“5 + 3”) of ZUSM every year. Therefore, multicenter studies (multiple medical schools) might be better to understand the perception, practice, and barriers of medical research among pediatric undergraduates. Even so, the findings in this study indicate that lack of time, lack of guidance, lack of training and limited English might be the common barriers to scientific work for pediatric undergraduates. Furthermore, the questionnaire for teachers and administrators would be performed to offer some concrete solutions in future.
Conclusions
Although pediatric undergraduates recognized the importance of medical research, interest and practices in research still require improvement. Lack of time, lack of guidance, lack of training and limited English were the common barriers to scientific work. Therefore, research training and English improvement were recommended for pediatric undergraduates.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- ZUSM:
-
Zhejiang University School of Medicine
- KMO:
-
Kaiser-Meyer-Olkin
References
Hanney SR, González-Block MA. Health research improves healthcare: now we have the evidence and the chance to help the WHO spread such benefits globally. Health Res Policy Syst. 2015;13:12.
Adebisi YA. Undergraduate students’ involvement in research: values, benefits, barriers and recommendations. Ann Med Surg (Lond). 2022;81:104384.
Petrella JK, Jung AP. Undergraduate research: importance, benefits, and challenges. Int J Exerc Sci. 2008;1(3):91–5.
Stone C, Dogbey GY, Klenzak S, Van Fossen K, Tan B, Brannan GD. Contemporary global perspectives of medical students on research during undergraduate medical education: a systematic literature review. Med Educ Online. 2018;23(1):1537430.
El Achi D, Al Hakim L, Makki M, Mokaddem M, Khalil PA, Kaafarani BR, et al. Perception, attitude, practice and barriers towards medical research among undergraduate students. BMC Med Educ. 2020;17(1):195.
Funston G, Piper RJ, Connell C, Foden P, Young AM, O’Neill P. Medical student perceptions of research and research-orientated careers: an international questionnaire study. Med Teach. 2016;38(10):1041–8.
Tatum M. China’s three-child policy. Lancet. 2021;397:2238.
Rivkees SA, Kelly M, Lodish M, Weiner D. The Pediatric Medical Student Research Forum: fostering interest in Pediatric Research. J Pediatr. 2017;188:3–4.
Barrett KJ, Cooley TM, Schwartz AL, Hostetter MK, Clapp DW, Permar SR. Addressing gaps in Pediatric Scientist Development: the Department Chair View of 2 AMSPDC-Sponsored Programs. J Pediatr. 2020;222:7–e124.
Jacobs CD, Cross PC. The value of medical student research: the experience at Stanford University School of Medicine. Med Educ. 1995;29(5):342–6.
Muhandiramge J, Vu T, Wallace MJ, Segelov E. The experiences, attitudes and understanding of research amongst medical students at an Australian medical school. BMC Med Educ. 2021;21(1):267.
Pop AI, Lotrean LM, Buzoianu AD, Suciu SM, Florea M. Attitudes and practices regarding Research among Romanian Medical Undergraduate Students. Int J Environ Res Public Health. 2022;19(3):1872.
Pallamparthy S, Basavareddy A. Knowledge, attitude, practice, and barriers toward research among medical students: a cross-sectional questionnaire-based survey. Perspect Clin Res. 2019;10:73–8.
Assar A, Matar SG, Hasabo EA, Elsayed SM, Zaazouee MS, Hamdallah A, et al. Knowledge, attitudes, practices and perceived barriers towards research in undergraduate medical students of six arab countries. BMC Med Educ. 2022;22(1):44.
Kharraz R, Hamadah R, AlFawaz D, Attasi J, Obeidat AS, Alkattan W, et al. Perceived barriers towards participation in undergraduate research activities among medical students at Alfaisal University-College of Medicine: a Saudi Arabian perspective. Med Teach. 2016;38(Suppl 1):S12–8.
Fournier I, Stephenson K, Fakhry N, Jia H, Sampathkumar R, Lechien JR, et al. Barriers to research among residents in Otolaryngology - Head & Neck surgery around the world. Eur Ann Otorhinolaryngol Head Neck Dis. 2019;136(3S):S3–7.
Abu-Zaid A, Alkattan K. Integration of scientific research training into undergraduate medical education: a reminder call. Med Educ Online. 2013;18:22832.
Eyigör H, Kara CO. Otolaryngology residents’ attitudes, experiences, and barriers regarding the Medical Research. Turk Arch Otorhinolaryngol. 2021;59(3):215–22.
Möller R, Shoshan M. Medical students’ research productivity and career preferences; a 2-year prospective follow-up study. BMC Med Educ. 2017;17(1):51.
Laidlaw A, Aiton J, Struthers J, Guild S. Developing research skills in medical students: AMEE Guide 69. Med Teach. 2012;34(9):e754–71.
Horwitz EK, Horwitz MBH, Cope J. Foreign Language Classroom anxiety. Mod Lang J. 1986;70(2):125–32.
Deng J, Zhou K, Al-Shaibani GKS. Medical English anxiety patterns among medical students in Sichuan, China. Front Psychol. 2022;13:895117.
Ma Y. Exploring medical English curriculum and teaching from the perspective of ESP-A case study of a medical English teaching. Technol Enhan Lang Educ. 2009;125(1):60–3.
Yan S, Huang Q, Huang J, Wang Y, Li X, Wang Y, et al. Clinical research capability enhanced for medical undergraduates: an innovative simulation-based clinical research curriculum development. BMC Med Educ. 2022;22(1):543.
Acknowledgements
The authors thank all the students who participated as volunteers for their contribution to the study.
Funding
This work was supported by grants from the “14th Five-Year Plan” teaching reform project of an ordinary undergraduate university in Zhejiang Province (jg20220041) and project of graduate education research in Zhejiang University (20210317).
Author information
Authors and Affiliations
Contributions
CZ designed and supervised the study progress. CZ and YZ wrote the manuscript and collected and analyzed the questionnaire data. All the authors have read and approved the manuscript prior to submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Our study was approved by the Ethics Review Committee of the Children’s Hospital of Zhejiang University School of Medicine and was undertaken according to the Helsinki declaration. Written informed consent was obtained from each participant upon their application to the work.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhan, C., Zhang, Y. Perception, practice, and barriers toward research among pediatric undergraduates: a cross-sectional questionnaire-based survey. BMC Med Educ 24, 364 (2024). https://0-doi-org.brum.beds.ac.uk/10.1186/s12909-024-05361-x
Received:
Accepted:
Published:
DOI: https://0-doi-org.brum.beds.ac.uk/10.1186/s12909-024-05361-x